Having discussions about end-of-life care preferences and recording and sharing these decisions with relevant health care professionals may influence your where you die, according to analysis of 21,231 UK urgent care register records. Martina Orlovic of The Royal Marsden NHS Foundation Trust and Imperial College London, UK, and colleagues present these findings in the open-access journal PLOS ONE on December 9, 2020.
Advance care planning gives patients the opportunity to discuss, express and document their wishes and preferences about future medical treatment and end-of-life care.The authors of the present study used the UK’s largest electronic palliative care register, Coordinate My Care, to analyze the anonymised recorded care preferences and place of death outcomes for 21,231 adults on this register who died between March 2011 and July 2019.
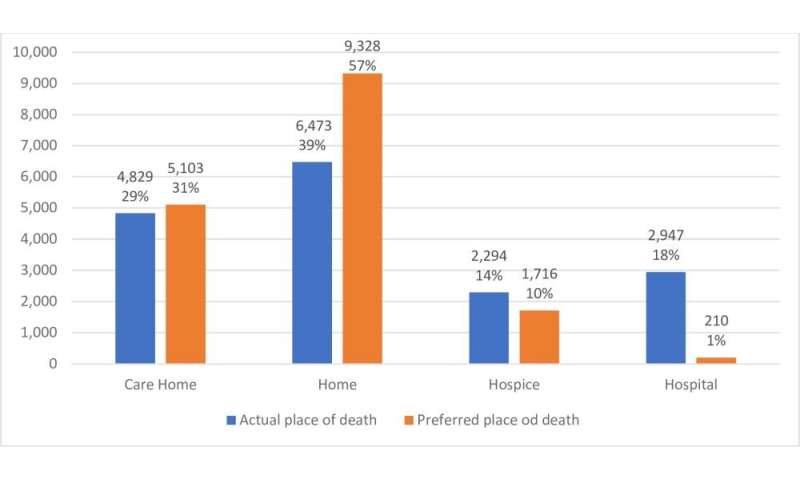
The researchers found that of the 16,593 individuals where both preferred place of death and actual place of death was recorded, 56 percent (9,328) preferred to die at home, while just 1 percent (210 individuals) wished to die in hospital. 73 percent of patients (12,171) died in their place of choice.
Across the whole cohort, which included individuals without a recorded place of death preference, 22 percent of individuals (4,626) died in hospital, with 78 percent dying in non-hospital settings, including at home (7,709, 36 percent) or in a care home (5,645, 27 percent).
The researchers note that patients without a recorded place of death preference were much more likely to die in hospital than those with a recorded preference (OR = 1.43, 95% CI 1.26-1.62, p<0.001). They also compared place of death with documented decisions about extent of appropriate medical intervention. IIndividuals with a documented decision not to be resuscitated in the event of cardio-pulmonary arrest were significantly less likely to die in hospital than those who were "for resuscitation" (OR = 0.43, 95% CI 0.37-0.50, p<0.001).
Although not all patients in this cohort were able to die in their place of choice, the authors conclude that advance care planning could help influence individuals’ end-of-life care experiences by facilitating patients, their families and clinicians to engage in discussions about their preferences for care. They note that the current COVID-19 pandemic highlights the need for health care professionals to discuss advance care planning with seriously ill patients.
Source: Read Full Article
