Does race play a role in how well someone recovers after stroke? New research focused on younger people who have had a hemorrhagic stroke found that young black and Latino people may be less likely than young white people to be disabled or even die within three months after a stroke. The new study is published in the January 22, 2020, online issue of Neurology, the medical journal of the American Academy of Neurology.
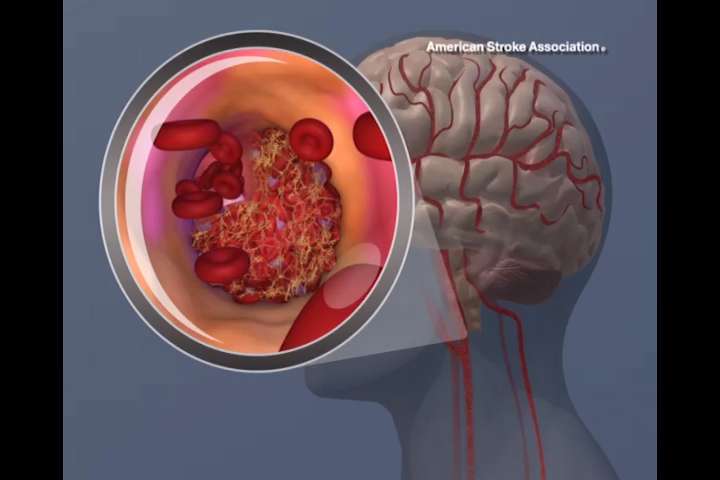
Hemorrhagic strokes, also known as bleeding strokes, happen when a blood vessel ruptures in the brain. They are much less common than ischemic strokes, when blood flow to the brain is blocked. They are also more difficult to treat and therefore more likely to be deadly.
“There has been considerable research on stroke in older people, but there is still much to be learned about stroke in younger people and how it affects people of different races and ethnicities,” said study author Daniel Woo, MD, MSc, of the University of Cincinnati in Ohio and a Fellow of the American Academy of Neurology. “Our study found that even when you account for factors that affect outcomes, such as how big the stroke is, race and ethnicity were still independent predictors of how well people would recover.”
The study involved 418 people with an average age of 43 who all had a bleeding stroke. Of the group, 173 were black people, or 41 percent, 197 were Latino people, or 47 percent, and 48 were white people, or 12 percent.
Researchers reviewed brain scans showing the size of the brain bleed in each person. They evaluated each person’s level of disability three months after stroke. Each person was assigned a score ranging from zero to six based on their level of disability.
Participants were divided into two groups. People in the first group had a score of zero to three, where zero meant no symptoms and three meant they had moderate disability but were able to walk without assistance. People in the second group, the poor outcome group, had a score of four to six, where four meant they had more severe disability and were unable to walk without assistance and six meant they had died.
A total of 52 percent of the white people were in the poor outcome group, compared to 35 percent of the black people and 31 percent of the Latino people.
When compared to white people, black people had a 58 percent lower risk of poor outcome and Latino people had a 66 percent lower risk. The results remained significant after adjusting for age, sex, blood pressure as well as the location and volume of the stroke.
“We examined both the initial size and the expansion of the bleeding in the brain for each participant when they were hospitalized, but were not able to find significant evidence that these factors contributed to how well they were doing three months later,” said Woo. “Therefore, these findings may indicate that the differences in outcome between black people, Latino people and white people may be driven more by biological, social and treatment factors related to the risk of bleeding stroke, rather than by differences in early management after admission to the hospital. For example, among our study participants, 8 percent of white people, or four people, had taken blood thinners prior to their stroke, compared to 4 percent of black people, or six people, and 1 percent of Latino people, or two people. Blood thinners are a known risk factor for bleeding stroke. However, these numbers are so small that more research is needed.”
Source: Read Full Article
