The latest guidance in addressing proper monitoring and reversal of neuromuscular blockade drugs during general anesthesia—a major advance in patient safety and satisfaction—was published today in Anesthesiology.
“Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade: A Report by the ASA Task Force on Neuromuscular Blockade” provide the American Society of Anesthesiologists’ (ASA) recommendations for managing and reversing neuromuscular blockade.
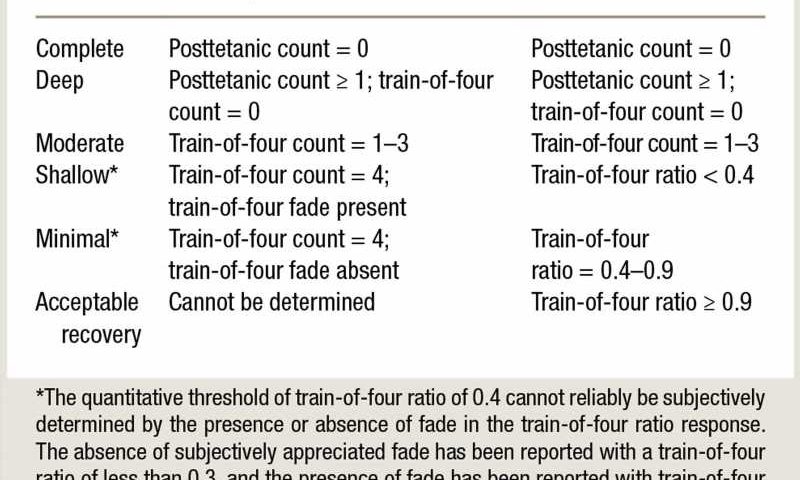
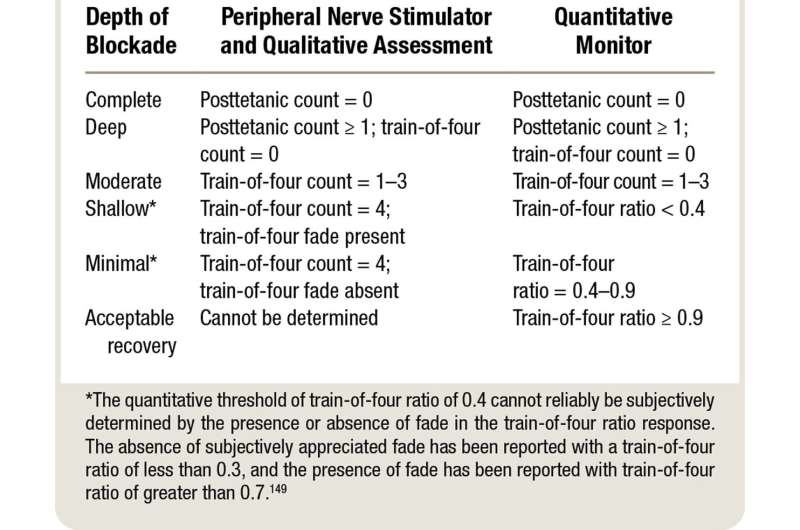
Neuromuscular blocking drugs, also known as muscle relaxants, are used after anesthesia is started to ease the insertion of a breathing tube in a patient’s windpipe, as well as relax the patient’s muscles to prevent movement. While these drugs aid surgery, it is important to prevent any lingering effect of the muscle relaxant—known as residual paralysis—after general anesthesia.
The new practice guidelines are intended to help anesthesiologists reduce the likelihood of residual paralysis and include recommendations for monitoring drug effects as well as effective approaches to adequately reverse muscle relaxation. Proper reversal of the effects of muscle relaxants helps reduce postoperative complications such as pneumonia, respiratory arrest, and reintubation, which can lead to increased time spent in the ICU and the hospital.
“ASA’s evidence-based practice guidelines for the management of neuromuscular blockade during surgery will help our members and increase the safety and satisfaction of our patients,” said ASA President Michael W. Champeau, M.D., FASA. “The clinical recommendations for monitoring and reversing this process will help prevent residual neuromuscular blockade so patients benefit from complete recovery, which may decrease the length of stay in the post-acute care unit (PACU) and postoperative lung complications.”
ASA’s practice guidelines are systematically developed recommendations to assist the physician and patient in making decisions about health care. These recommendations may be adopted, modified, or rejected according to clinical needs and constraints and are not intended to replace local institutional policies. In addition, practice guidelines developed by the ASA are not intended as standards or absolute requirements, and their use cannot guarantee any specific outcome.
Practice guidelines are subject to revision as warranted by the evolution of medical knowledge, technology, and practice. They provide basic recommendations for anesthesia care that are supported by synthesis and analysis of current literature, expert and practitioner opinion, public comment, and clinical feasibility data. Practice guidelines aim to improve patient care and patient outcomes by providing up-to-date information for patient care.
More information:
Stephan R. Thilen et al, 2023 American Society of Anesthesiologists Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade: A Report by the American Society of Anesthesiologists Task Force on Neuromuscular Blockade, Anesthesiology (2022). DOI: 10.1097/ALN.0000000000004379
Journal information:
Anesthesiology
Source: Read Full Article