The successful campaign of adoptive T cell therapies, a type of immunotherapy in which immune T cells are collected from a patient, enhanced outside of the body, and reinfused back into the same patient, especially against blood cancers is well under way. But improving the ability to create patient-specific T cell populations with specific traits and functions could broaden clinicians’ repertoire of T cell therapies.
One way to approach this goal is to better understand how T cells’ traits and functions, including their cytotoxic effects on unwanted target cells (effector T cells) or their ability to recall and eliminate them if they show up again (memory T cells), are shaped by the mechanical resistance of the tissues they encounter while infiltrating them. The mechanical features of tissues, for example, bone, muscle, different internal organs, and blood, can vary widely, and pathological tissues such as tumor masses or fibrotic tissues are mechanically significantly different from healthy tissues.
Now, a research team at the Wyss Institute for Biologically Inspired Engineering at Harvard University and Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS), led by Wyss Core Faculty member David Mooney, Ph.D., took a novel biomaterials approach to investigate the effect of tissue mechanics on the state of T cells.
By engineering a 3-dimensional model of the extracellular matrix (ECM), produced by cells that are responsible for tissues’ different stiffnesses and viscoelasticities, they were able to tune both parameters independently. This enabled them to demonstrate a distinct impact of tissue viscoelasticity on T cell development and function in vitro and in vivo, and to identify a molecular pathway driving the phenomenon. The findings are reported in Nature Biomedical Engineering.
Mechanical resistance comes in the form of “stiffness,” a tissue’s (or any material’s) resistance to instantaneous deformation, and “viscoelasticity,” the type of relaxation it exhibits over time following its deformation. Explained in physical terms, a viscous (fluid) material, like honey, is more likely to flow, while an elastic (solid) material returns more rapidly to its original shape, like a rubber band after stretching—and this holds true for tissues which are composed of both solid and fluid components.
“Importantly, the phenotypes, functions, and gene expression programs of T cells trained in variations of the system correlated well with those we found in T cells in mechanically distinct tissues from patients with cancer or fibrosis,” said Mooney who also is the Robert P. Pinkas Family Professor of Bioengineering at SEAS, and leads the Wyss Institute’s Immunomaterials Initiative. “Our study provides a conceptual basis for future strategies aiming to create functionally distinct T cell populations for adoptive therapies by selectively tuning mechanical input provided by biomaterials-based engineered cell culture systems.”
Mimicking tissue mechanics in a dish
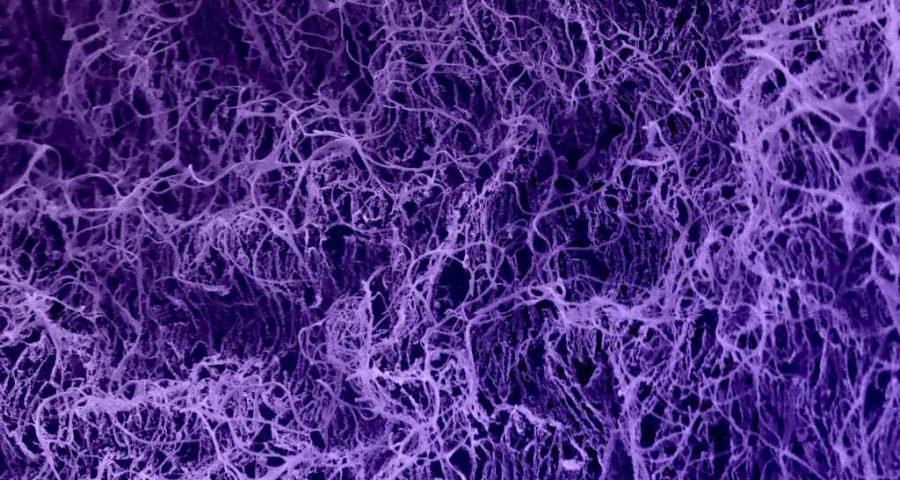
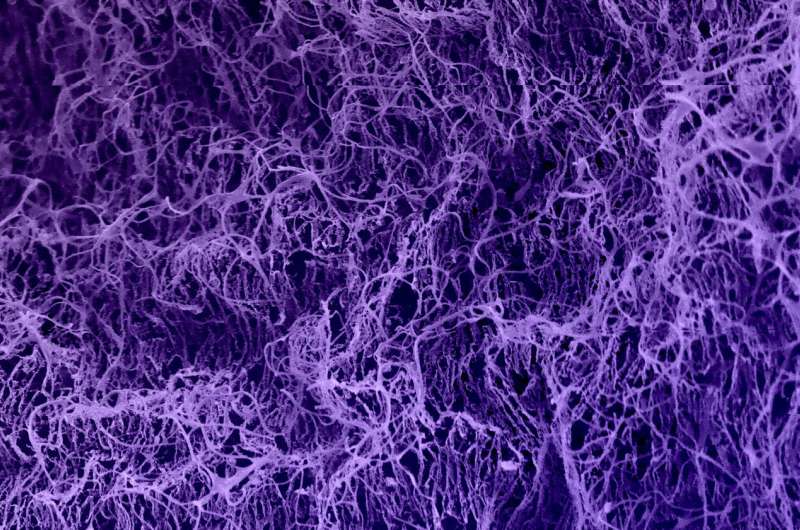
Key to their discoveries was the team’s engineering of a tunable ECM model, in which they focused on a type of collagen that they found to be key to dictating the mechanical behavior of different tissues. Collagen is a major ECM protein secreted by almost all cells in the body. Individual collagen protein molecules are naturally organized into crimped fibrils that aggregate further into fibers by chemically cross-linking themselves. Each fibril can be considered a mechanical spring, and each fiber as an assembly of springs. An ECMs stiffness depends on how densely it is packed with collagen molecules, whereas its distinct viscoelasticity depends on how densely collagen molecules are cross-linked to each other.
To mimic natural collagen-based ECM, the team fabricated hydrogels whose stiffness they could tune by varying the concentration of collagen molecules: fewer numbers of collagen molecules produced lower stiffness and higher numbers, higher stiffness. Independently, viscoelasticity became tunable by varying the amounts of a synthetic cross-linker molecule that further networked the collagen molecules. More highly cross-linked collagen molecules produced more elastic hydrogels. The resulting ECM-mimicking hydrogels equally allowed the attachment of pre-activated T cells but, importantly, enabled their stimulation with specific mechanical signals.
“To our knowledge, this is the first ECM model that allows researchers to study T cells with stiffness from viscoelasticity decoupled, and thus enables us and others in the future to investigate how immune and other cells might be mechanically regulated,” said co-first author Yutong Liu, Ph.D., who was a graduate student in Mooney’s group. “The system’s defined and uniform mechanical stimulation is vastly different from how T cells are usually cultured—cells that attach to the bottom of a culture dish encounter a highly inelastic surface, while those remaining in suspension are surrounded by the viscous medium.”
Natural consequences of mechanical action
The team performed an extensive analysis of T cells exposed to different viscoelastic conditions. “T cells that experienced a more elastic collagen matrix were more likely to develop into ‘effector-like T cells,’ whereas T cells that experienced a more viscous ECM matrix rather became ‘memory-like T cells,'” said co-first author Kwasi Adu-Berchie, Ph.D., who completed his Ph.D. in Mooney’s lab and is currently a Translational Immunotherapy Scientist at the Wyss Institute.
“Importantly, we found that a T cell’s state, resulting from the viscoelasticity of a matrix, even more so from more elastic, less viscous hydrogels, becomes long-term imprinted, as the cell retains a memory of that specific matrix after being transferred to a different one. This could have broad implications for future cell manufacturing.”
Gene expression analysis led the team to the activity of a transcription factor known as AP-1 that links T cells’ reception of a more elastic, less viscous mechanical environment to a more effector-like gene expression program. The number of AP-1 complexes with specific compositions was increased, and genes depending on them for their expression were enriched, not only in T cells isolated from more elastic hydrogels, but also in T cells isolated from patients’ cancer and fibrotic tissues, which are stiffer and more elastic than neighboring healthy tissues. When they inhibited one of AP-1’s components with a drug, the effects of a more elastic collagen matrix on T cells were prevented.
To investigate how different mechanical stimulations and T cells’ predicted gene expression signatures translated into actual traits and functions, the team used therapeutic CAR-T cells engineered to bind a specific antigen of a human lymphoma cell line. CAR-T cells that were stimulated in a more elastic collagen matrix in vitro exhibited a stronger ability to kill lymphoma cells. Also in vivo, CAR-T cells stimulated in a more elastic matrix, and adoptively transferred into mice with the same type of lymphoma, were significantly more capable of reducing tumor burden in the animals and extending their lives than CAR-T cells exposed to a less elastic matrix.
“This study merges three seemingly disparate fields, biomaterials, immunotherapy, and mechanobiology, to develop an entirely new form of biomaterials-based mechanotherapeutic. It is easy to see how these findings can potentially open up new avenues to improve adoptive T cell therapies for patients in the future,” said Wyss Founding Director Donald Ingber, M.D., Ph.D., who is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital, and the Hansjörg Wyss Professor of Bioinspired Engineering at SEAS.
More information:
Generation of functionally distinct T-cell populations by altering the viscoelasticity of their extracellular matrix, Nature Biomedical Engineering (2023).
Journal information:
Nature Biomedical Engineering
Source: Read Full Article