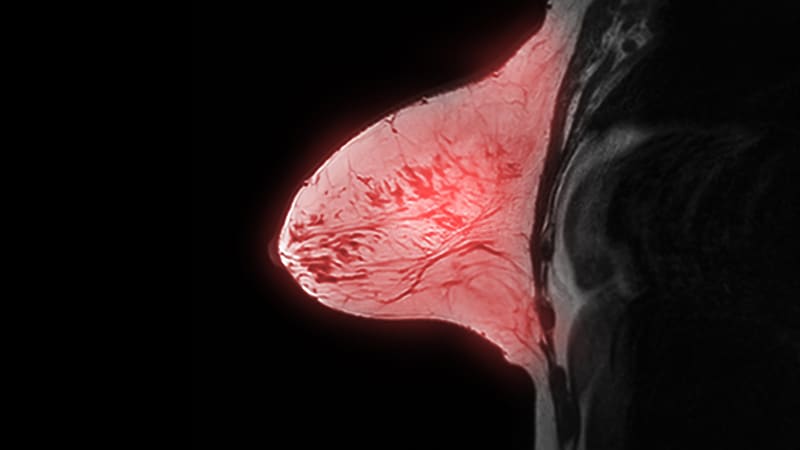
BOSTON — Having a preoperative MRI scan does not help surgeons to reduce the likelihood of positive surgical margins when they are performing lumpectomy for early-stage breast cancer, a new study concludes.
The current results suggest that MRI is “not useful to achieve this goal and not a productive use of healthcare resources,” said senior author Marissa Howard-McNatt, MD, director of the Breast Care Center, Wake Forest University, Winston-Salem, North Carolina.
“Researchers continue to look for better ways to assess margin status while the patient is still on the operating table,” she said, as a re-operation “can be traumatic.”
The study will be presented at the 24th American Society of Breast Surgeons (ASBrS) Annual Meeting on April 28, and was highlighted in a press briefing.
In the study, more than 630 patients with early stage breast cancer were randomly assigned to partial mastectomy with or without cavity shaving of the tumor margins, of whom 193 underwent MRI prior to their operation.
Although there was a difference in the rate of positive surgical margins before cavity shaving between patients who did and did not undergo MRI, the difference did not reach statistical significance.
“MRI exams are costly and potentially stressful for patients,” Howard-McNatt commented in a press statement. “The thought is that they will help physicians achieve negative margins during the initial surgery. However, our study shows this is simply not the case.”
Approached for comment, Mediget Teshome, MD, MPH, said, “In my practice, I primarily utilize MRI preoperatively to evaluate the extent of disease in cases where the information is not clear from mammogram and ultrasound.”
This may be when there is “discordance between the size of the malignancy or concern for chest wall or muscle involvement,” Teshome told Medscape Medical News.
MRI is also useful when there may be occult disease, such as in patients “with high suspicion for extensive intraductal component not evident on mammography and those who present with axillary metastasis and unknown breast primary,” as well as in high-risk patients with a genetic predisposition for breast cancer, she explained.
However, Teshome, an associate professor in the Department of Breast Surgical Oncology at the University of Texas MD Anderson Cancer Center in Houston, stressed that, “as with any test, it is important that preoperative MRI is performed with the specific intent to inform clinical decision making in a meaningful way.”
“While it can provide a benefit in selected cases given its high sensitivity, MRI is associated with false positives and can also contribute to increased patient anxiety and additional procedures,” she cautioned.
Study Details
Lumpectomy has become “a mainstay of breast cancer management, with safe and reliable outcomes as compared to mastectomy,” said Howard-McNatt, but it is associated with a higher rate of positive margins, of up to 27%.
She underlined that “re-excision surgery can contribute to greater morbidity, patient anxiety, poor cosmetic outcomes, and healthcare system overload,” and the desire to reduce re-operations has led to “much attention” being paid to preoperative imaging.
Their study set out to investigate the value of preoperative MRI in this regard, and for this they analyzed data on 631 women who had who had participated in two prior randomized trials (SHAVE1 and SHAVE2).
These women were randomly assigned to standard partial mastectomy with or without resection of cavity shave margins, with preoperative MRI performed prior to randomization in both trials at the surgeon’s discretion.
The median tumor size was 1.3 cm. An extensive intraductal component was identified in 32.8% of patients, 26.1% had palpable tumors, and 7% had invasive lobular histology. Neoadjuvant chemotherapy was administered in 6.5% of patients.
In all, 193 individuals underwent MRI. These women were less likely to have a positive surgical margin before resection of cavity shave margins, at 31.1% vs 38.8% in those who did not have MRI, although the difference was not statistically significant (P = .073).
Multivariate analysis taking into account patient age, race, receipt of neoadjuvant chemotherapy, the presence of an extensive intraductal component, as well as histologic subtype and tumor size, revealed that MRI was not associated with a higher rate of negative surgical margins (P = .110).
However, it was shown that both tumor size (P = .040) and age (P = .032) were predictive of margin status.
It was notable that MRI use was associated with younger patient age, at a median of 63 years vs 66 years, and smaller tumor size, at a median of 2.0 cm vs 2.1 cm.
This latter finding “may be attributable to an inaccurate initial assessment of the extent of the actual tumor size for a variety of reasons,” Howard-McNatt commented. “For example, tumors may be discontinuous or have satellite lesions which may touch the edge of a specimen.”
The study was funded in part by the David and Katie Burke Fund for Breast Cancer Research, the Connecticut Breast Health Initiative, the Troy Cancer Program, Cleveland Clinic Akron General Operations, the Cleveland Clinic Akron General Foundation, the Lineberger Comprehensive Cancer Center, the Watson Clinic Center for Research Inc., and LifeCycle. The study authors report no relevant financial relationships.
24th American Society of Breast Surgeons Annual Meeting: Abstract 1380029. Presented April 28, 2023
For more from Medscape Oncology, join us on Twitter and Facebook
Source: Read Full Article