In a pilot study of 44 Major League Baseball pitchers, an MRI view of the elbow using a new positioning protocol improved diagnosis of injuries to the ulnar collateral ligament compared with a standard MRI view.
Acute and chronic injuries to the ulnar collateral ligament (UCL) are common in throwing athletes because of the repetitive extreme valgus stress caused by overhead throwing; however, accurate assessment of UCL injuries using standard MRI remains a challenge, noted Pamela J. Lund, MD, of SimonMed Imaging, Mountain View Hospital, Las Vegas, Nevada, and colleagues.
“This difficulty in part relates to suboptimal rendering of the UCL on the imaging planes obtained from conventional patient positioning for elbow MRI,” but the incorporation of elbow valgus stress into an MRI imaging procedure has not been well studied, the investigators write.
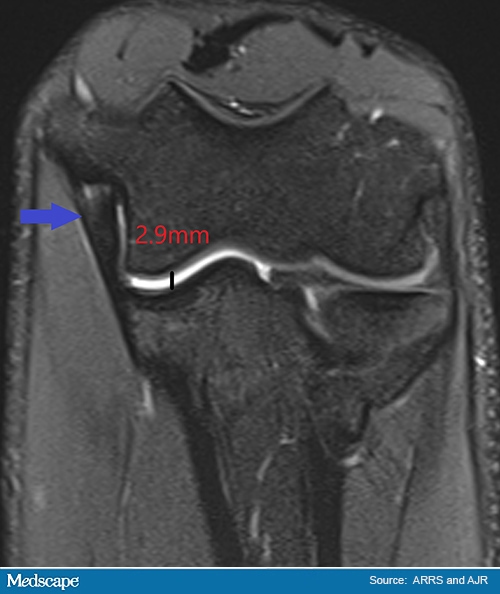
The FEVER view in MRI.
In the study, published June 2 in the American Journal of Roentgenology , the researchers compared standard MRI view with what they call the “flexed elbow valgus external rotation (FEVER) view” on ulnotrochlear (UT) joint space measurement. The pilot study included 44 Major League Baseball pitchers who ranged in age from 18-36 years. All were men, 16 were symptomatic at the time of the MRI, and 6 had undergone previous UCL reconstruction.
Overall, the FEVER view yielded an average increase of 1.80 mm in UT joint space width. FEVER view also increased confidence in UCL-related findings, as two independent radiologists identified three and two abnormalities in the UCL using the FEVER view that were not apparent on a standard view. Intrareader agreement for UT joint space measurement was higher for FEVER views compared with the standard view, with intraclass correlation coefficients of 0.92 and 0.54, respectively. Overall confidence increased by 1.09 for one reader and 0.77 for the second reader.
Positioning for the FEVER view was comfortable for most participants, the researchers noted. A total of 29 reported no pain during the procedure; 11 had pain scores of 1-3, four had scores of 4-7, and none had scores above 7.
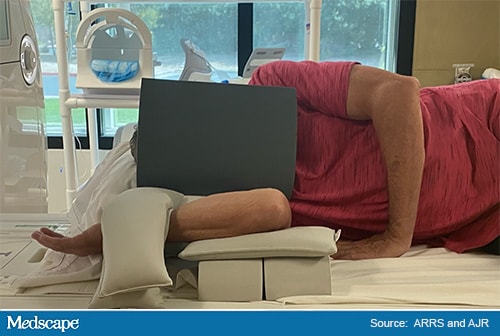
Positioning for the FEVER view.
The FEVER view involved positioning of the patient lying on the affected arm in the lateral decubitus position. The shoulder and elbow were flexed to 90 degrees with the palm facing up, and the elbow was elevated approximately 4 inches from the table on top of two foam pads and a sandbag. Two additional sandbags were used to produce valgus stress and immobilization.
The study findings were limited by the pilot design and small sample size. However, the results suggest that the FEVER view may improve evaluation of UCLs for throwing athletes, the researchers concluded.
The goal of the prospective pilot study was to use a new elbow MRI view and patient position “designed to achieve reproducible valgus stress across the ulnotrochlear joint to evaluate the UCL in throwing athletes,” Lund said in an interview with Medscape Medical News. “We used a 30%-35% angle from horizontal,” she noted. Some features visible on the FEVER stress view in one patient included a more elongated ligament, Lund noted. In another patient, the FEVER view identified a partial tear as well as a sprain, compared with the standard image that only identified the sprain, she said.
“The FEVER view is practical, reproducible, and well-tolerated by throwing athletes,” said Lund. However, “We will need further studies including the nonthrowing elbow, and clinical performance correlation to determine the absolute diagnostic utility of the FEVER view,” she concluded.
FEVER View Optimizes Options
“UCL injuries are increasing in number, and at an earlier age, and imaging is a big part of the management of this injury,” said John Wilckens, MD, a sports medicine specialist at Johns Hopkins University, Baltimore, Maryland, told Medscape Medical News.
Wilckens, who was not involved in the study, said he was not completely surprised by the study findings. “I thought it was interesting that both symptomatic and asymptomatic patients had similar joint laxity on the FEVER series,” he said. “Also, asymptomatic had less peri-ligamentous edema, suggesting that the positioning may ‘wring out the edema’ to some extent,” he noted. He said he was somewhat surprised by how well patients tolerated the FEVER series, with manageable levels of discomfort in most cases.
“I think it is always best to examine an injured structure as close to the position of symptoms as possible, to try to reproduce a dynamic phenomenon in a static image,” Wilckens noted. “The FEVER sequences seem to capture the ligament well, at least in the images in this study.”
However, he added, “I would caution that laxity does not always equal pathology. I know there would be some value to use it as a crystal ball, but it is more of a fossil record, which also has some clinical value.”
Potential barriers to the routine use of FEVER could be the discomfort of the positioning, “especially in the acutely injured elbow and in elbows with arthritis or limited range of motion,” Wilckens noted. “The study authors appropriately identify that the shoulder position may influence elbow imaging.”
Overall, “This is an interesting concept that should be further tested on additional throwers,” said Wilckens. Areas for further study include whether an injection into the elbow would augment their findings, he said. “It would be interesting to repeat this study in skeletally immature throwers as well.”
“MRI and MR arthrography are highly accurate ways to evaluate soft-tissue structures about the elbow, including the ulnar collateral ligament, which is important for elbow stability in throwers,” said Jan Fritz, MD, chief of musculoskeletal radiology at NYU Grossman School of Medicine, New York City, in an interview with Medscape Medical News.
“However, MRI and MR arthrography are usually performed statically with the arm extended and, notably, without exerting diagnostic valgus stress on the medial side of the elbow. Valgus stress can help diagnose instability by the dynamic widening of the medial joint space and nondisplaced ligament tears, indicating impairment of the elbow-stabilizing ulnar collateral ligament,” Fritz explained.
“Stress radiographs and dynamic stress ultrasound examinations are usually used to supplement MRI,” said Fritz, who was not associated with the FEVER study. “MRI in standard position and with the proposed FEVER position can add this valgus stress component to MRI exams and potentially increase the performance of detecting ulnar collateral ligament injuries and medial elbow joint destabilization. However, overall, the differences were less than 5%, and there was no standard of reference to indicate which technique is more accurate.”
More studies would be needed to confirm the findings with an appropriate standard of reference, he emphasized.
“The FEVER position requires more complex orientation of the elbow on the MRI table compared to standard MRI,” Fritz noted. “Both the repositioning during the MRI examination and the acquisition of the FEVER images prolong the total duration of the exam.”
Although the longer duration was feasible in a prospective, standardized study setting, “the feasibility in clinical practice and the required learning curve are currently unknown,” he added. Most participants tolerated FEVER position well, but “some participants experienced mild-to-moderate discomfort, which may result in motion during MRI acquisition and degradation of image quality,” Fritz said.
“Additional research is required to understand whether the small differences in detection rates of abnormal MRI findings on standard views and FEVER view can reach statistical significance,” said Fritz. More research is also needed, he asserted, to confirm which view is more accurate “by understanding whether higher detection rates of abnormalities represent false-positive or true-positive results and understanding whether the detected abnormalities are clinically meaningful and positively influence treatment and surgical decision-making.”
The study received no outside funding. Wilckens and the study authors have disclosed no relevant financial relationships. Fritz disclosed research support from Siemens AG, BTG International, Microsoft Corporation, Zimmer Biomed, DePuy Synthes, QED, SyntheticMR, and has previously and/or currently served as a scientific advisor to Siemens AG, SyntheticMR, General Electric Healthcare, QED, BTG, ImageBiopsy Lab, Boston Scientific, and Mirata Pharma.
Am J Roentgenol. Published online June 2, 2021. Full text
Heidi Splete is a freelance medical journalist based in Washington, DC.
For more news, follow Medscape on Facebook, Twitter, Instagram, YouTube, and LinkedIn
Source: Read Full Article