Genomic sequencing may provide a way to refine stratification for adjuvant therapy for patients with resected localized clear-cell renal cell carcinoma (ccRCC), according to a new study.
In a study of tissue samples from more than 900 international patients with ccRCC, tumors with von-Hippel Lindau (VHL) mutation alone were associated with the most favorable outcomes at 5 years.

Dr Yasser Riazalhosseini
“We have established a new way of personalizing healthcare for patients with renal cell carcinoma using genomic information about their specific tumor,” study author Yasser Riazalhosseini, PhD, assistant professor of human genetics and head of cancer genomics at the Victor Phillip Dahdaleh Institute of Genomic Medicine at McGill University, Montreal, Canada, told Medscape Medical News.
The study was published February 23 in Clinical Cancer Research.
Mutations and Recurrence
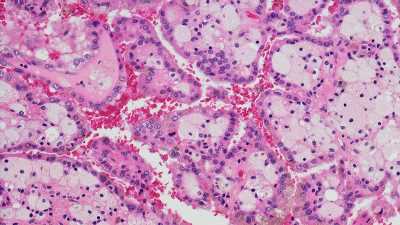
The most common type of kidney cancer, accounting for 70% to 80% of cases, is ccRCC. Some patients with resected ccRCC remain at risk for recurrence. Determining this risk is often problematic for clinicians.
In the current study, the researchers examined whether genetic mutations play a role in determining this risk. The researchers determined the somatic mutation status of 12 genes in 943 ccRCC tumor samples that were taken from an international cohort. This cohort included patients from the United Kingdom, the Czech Republic, Romania, Russia, and Serbia. To examine the associations between mutation status and outcomes, the researchers created a discovery cohort (n = 469 patients) and a validation cohort (n = 474 patients).
They found that tumors that contained the VHL mutation alone were associated with significantly improved outcomes, compared with tumors that contained the VHL mutation plus additional mutations. This association was observed in both cohorts.
In the discovery cohort, among patients with VHL+0 tumors, the 5-year disease-free survival (DFS) rate was 90.8%. Among those with VHL+1 tumor, the DFS rate was 80.1%. Among patients with VHL+2 tumors, the DFS rate was 68.2%, and among those with VHL+>3 tumors, the DFS rate was 50.7%. This trend was replicated in the validation cohort.
Among patients eligible for adjuvant therapy, 29% had VHL+0 tumors. The 5-year DFS rate in this group was 79.3%. These patients could potentially be spared further treatment, the researchers write.
Among patients with VHL+2 and those with VHL+≥3 tumors, who made up 32% of those eligible for adjuvant therapy, DFS rates were equivalent (45.6% and 35.3%, respectively). These patients should be prioritized for adjuvant therapy, according to the authors.
“This study establishes the ability to define biologically distinct molecular subgroups of ccRCC that could be used to better inform patients and their physicians regarding individual risk of tumor recurrence following nephrectomy,” said Riazalhosseini.
Validation Needed
Commenting on the study for Medscape, Toni K. Choueiri, MD, director of the Lank Center for Genitourinary Oncology at Dana Farber Cancer Institute and Jerome and Nancy Kohlberg Professor of Medicine at Harvard Medical School in Boston, said, “This study builds on prior knowledge of renal cell carcinoma genomics and clonality. It is a large study, and tumors are taken from a single tumor region, so it is a practical study.” Choueiri did not participate in the research.

Dr Toni Choueiri
The risk stratification adds to the tumor-node-metastasis staging and other clinical prognostication systems, but certain observations must be made, he said. “Other features, like copy-number alterations, were not considered. Also, a higher risk of recurrence does not necessarily mean a benefit from adjuvant therapy. To that end, it will be interesting to see the immune tumor microenvironment of VHL+2 and VHL+≥3. A very important next step will be validation in a large, prospective adjuvant study.”

Dr Brandon Manley
Brandon J. Manley, MD, associate member in the Department of Genitourinary Oncology at Moffitt Cancer Center in Tampa, Florida, told Medscape that having data that enable one to estimate a patient’s risk of recurrence is “nice, but it doesn’t answer other critical questions, like who is going to respond and who is not going to respond.
“The study helps refine the clinical predictive algorithm using some fairly straightforward genomics, but it doesn’t really touch upon any of the sensitivity to the adjuvant treatment that we would give. Right now, there is only one, pembrolizumab. Nor did they take into account any of the personal decisions that come into play for patients beyond their genomics, such as other medical comorbidities and ability to tolerate such treatment,” he added. The clinical utility of these data is unclear, Manley concluded.
The study was supported by the EU FP7 and grants from Génome Québec; le Ministère de l’Enseignement supérieur, de la Recherche, de la Science et de la Technologie Québec; the Cancer Research Society; the Kidney Foundation of Canada; and McGill University. Riazalhosseini received grants from the Cancer Research Society, the Kidney Foundation of Canada, and Fonds de recherche du Québec – Santé during the conduct of the study. Choueiri and Manley reported no relevant financial relationships.
Clin Cancer Res. Published February 23, 2023. Abstract
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article