Leaders from the U.S. Department of Health and Human Services (HHS) visited the Washington University Medical Campus on Sept. 20 to learn about strategies to address the opioid crisis, which has claimed the lives of more than 200,000 people in the United States since 1999.
The visit helped launch a government public education campaign on the dangers of substance abuse. It also coincided with an announcement from Health and Human Services that the federal government will give states $1 billion to fight opioid addiction, including $44 million to the state of Illinois and $29 million to Missouri.
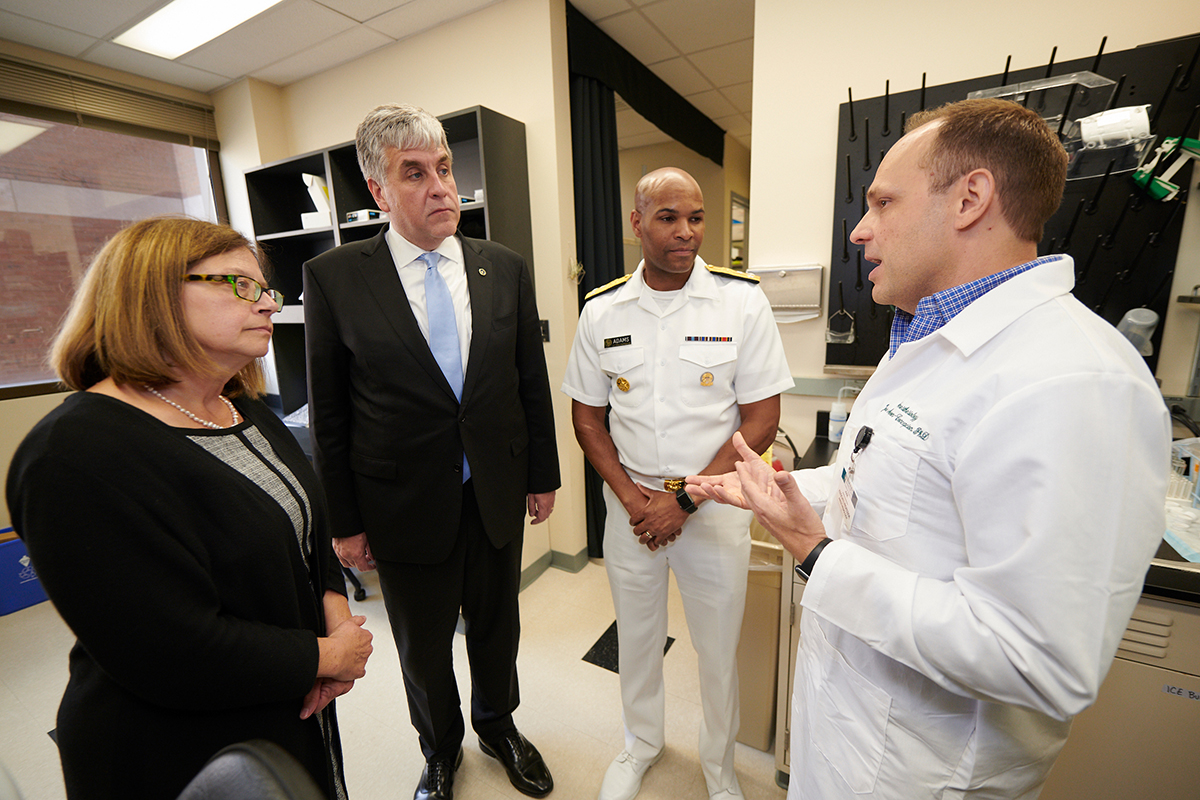
Eric D. Hargan, HHS deputy secretary, led a roundtable discussion, accompanied by U.S. Surgeon General Jerome M. Adams, MD, and Elinore F. McCance-Katz, MD, PhD, assistant secretary for mental health and substance use.

Participants included local leaders on the front lines of fighting the opioid crisis, including those from community organizations, law enforcement and health-care providers. Washington University addiction specialist Evan Schwarz, MD, an associate professor of emergency medicine and director of the Outpatient Medical Toxicology and Addiction Medicine Clinic, and Clay Dunagan, MD, BJC HealthCare senior vice president and chief clinical officer, represented the Medical Campus during the roundtable.
“This is the number one public health issue in the United States,” said Hargan, who was born in Cape Girardeau, Mo, and raised in nearby Southern Illinois. “For three years in a row, life expectancy has declined, and those declines are entirely due to opioids.”
A number of researchers at the School of Medicine are focused on understanding opioid addiction and chronic pain. The HHS leaders toured the laboratory of one of those researchers, Jose Moron-Concepcion, PhD, associate professor of anesthesiology.
His work focuses on understanding how opioids affect the brain. He and his colleagues have found that long-term opioid use seems to flip a switch in the brain that triggers cravings for months after drug use stops — an experience that can contribute to relapse. His research could lead to more effective ways to fight addiction.
“There are certain areas of the brain that respond to the repeated use of opioids,” Moron-Concepcion said. “If there is a way to break that cycle between opioid use and cravings, we may be able to help drug users and prevent relapse.”
On average, more than 134 people in the United States die each day from opioid overdoses, according to the U.S. Centers for Disease Control and Prevention. Opioid misuse and addiction — involving prescription pain relievers, heroin or synthetic opioids, such as fentanyl — are estimated to cost the U.S. economy more than $78 billion a year, in health-care costs, lost productivity, addiction treatment and criminal justice expenses.
During their visit to the Medical Campus, Hargan and Adams also met with David H. Perlmutter, MD, the George and Carol Bauer Dean of the School of Medicine, the Spencer T. and Ann W. Olin Distinguished Professor and the executive vice chancellor for medical affairs; Jennifer K. Lodge, PhD, vice chancellor for research; John P. Lynch, MD, a professor of medicine and vice president and chief medical officer at Barnes-Jewish Hospital; and Richard J. Liekweg, BJC HealthCare president and CEO.
They discussed the roots of the opioid crisis and research underway at the School of Medicine to develop alternatives to opioids for treating patients with chronic pain. They also discussed ways to promote cooperation among health-care providers in the St. Louis region regarding addressing addiction and mental health issues in opioid users.
“We are providing more training so that our physicians and trainees are better equipped to deal with these terrible problems involving opioids,” said Perlmutter. “But health-care providers can’t solve this problem alone, so we’re working to develop partnerships with law enforcement and social service agencies to address the needs of the opioid users.”
“As many people know, this issue is personal for me,” said Adams, the surgeon general. “I have a brother who currently is in prison because of his addiction. The number of overdose deaths is daunting — someone in the U.S. dies from opioids every 11 minutes — but we’re beginning to make progress. And by bringing together the people with the expertise to fight the problem, we think we can do better. We have to do better.”

Media Contact
Judy Martin Finch, Director of Media Relations
314-286-0105
Writer
Jim Dryden, Director of Broadcast & Podcasts
Jim Dryden covers psychiatry and neuroscience, orthopedics, diabetes, obesity and nutrition. He has a bachelor’s degree in English literature from the University of Missouri-St. Louis.
314-286-0110
Source: Read Full Article
