The UK Prescribing Safety Assessment (PSA) is a medical exam with strong stakeholder support and is associated with increased confidence in prescribing and decreased reporting of medication-related patient harm. The PSA is a joint initiative by the British Pharmacological Society (BPS) and Medical Schools Council (MSC) created to address findings in the first decade of this century that prescribing errors were common among junior doctors.
The use of medicines saves many lives but is also associated with harm. Some of these avoidable harms come from prescription errors, estimated to be present in up to one in every ten hospital prescriptions. The UK PSA is a targeted education initiative to prioritize patient safety.
It is a national exam that all medical students or doctors entering NHS clinical practice after medical school must pass, to demonstrate that they can prescribe medicines to patients safely. Although most UK medical students will pass the exam before becoming doctors, it is currently not mandated until the end of the first year of clinical practice in the NHS. This means that some newly qualified prescribing doctors have not yet passed this exam at present.
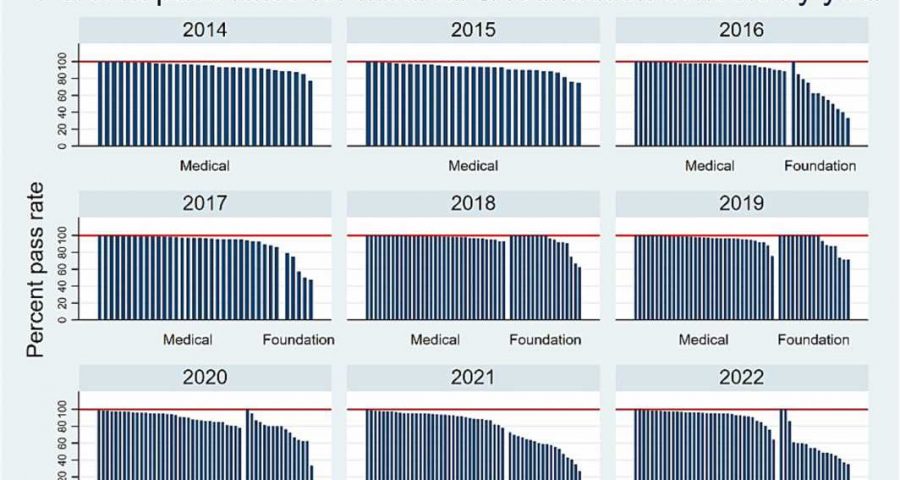
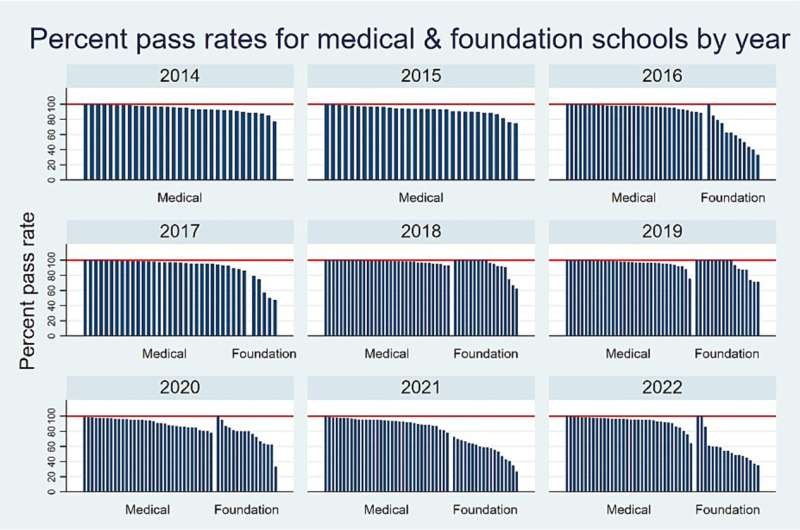
A review by Professor Dame Jane Dacre of the first decade of implementation of this exam, taken by more than 80,000 medical students and doctors, has found that students and educators think the assessment has driven more and better prescribing education and has been accompanied by trends that suggest NHS prescribing may now be safer. In what would be a major paradigm shift, the review recommended that all clinicians should be required to pass the exam prior to prescribing for patients in clinical practice.
Because this recommendation would require a shift in medical education nationally, a parallel study was undertaken to put all the exam information provided to the Dacre review into the public domain.
This study is now published in the British Journal of Clinical Pharmacology. The analysis of 10 years of data shows that the PSA is a good test that measures how prepared someone is to prescribe. It is a reliable and efficient exam, and provides a national standard, which the vast majority of UK medical students will pass (>90%) prior to working in the NHS.
The study supports the Dacre Review recommendations that passing the PSA should be a requirement for newly qualified medical practice in the UK, so that the NHS can continue to prioritize patient safety and ensure an appropriate threshold of experience prior to prescribing for patients.
Dame Jane Dacre, emeritus professor of medical education UCL, said, “Prescribing safety is essential to protect patients. Our review recommends that assessment of prescribing is best done before doctors qualify, so that relevant education, training and assessment happens before they are expected to prescribe for patients. Addition of the PSA to medical school finals would give new doctors better competence and confidence in safe prescribing.”
James Titcombe, patient safety advocate, said, “Safe prescribing is key to patient safety and has the potential to reduce medical error which can be costly to the lives of patients, as well as being a financial burden for health care systems. I welcome both the study and report, which highlight the importance of up-to-date knowledge of safe prescribing, and the consistency of applying that knowledge when prescribing to patients. The PSA is the key to ensuring better patient safety for all, which should be a health care priority for all involved in the prescribing of medicines.”
Dame June Raine DBE, chief executive of the Medicines and Health care products Regulatory Agency (MHRA) said, “Innovative medicines have brought hope to many patients for whom treatment options were previously unavailable. As medicines become more powerful and complex, safe prescribing by health care professionals plays an even more vital role. A prescriber must have a detailed knowledge of a medicine’s indication, dose, and potential adverse reactions.
“Now more than ever, all prescribers have a duty to proactively stay up to date with the constantly-evolving risks and benefits of medicines in clinical use. This includes playing an active role in reporting suspected side effects to the MHRA’s Yellow Card scheme to ensure adverse reactions are recorded and appropriate action is taken. Safe prescribing is a professional duty, and I therefore welcome the recommendations of this timely report.”
Professor Simon Maxwell, the PSA medical director, said, “Prescribing medicines is the most important means by which health care professionals treat illness, alleviate symptoms and prevent future ill health. Given the complexity of the task, it is inevitable that mistakes will occur, but minimizing them should be a key priority for improving the quality of health care delivery.
“This research demonstrates that developing the first national assessment of basic competence to prescribe has encouraged greater emphasis on training to undertake this important task. I am pleased to see that the Dacre review recommends extending this principle to all new doctors entering the NHS and believe that this will drive future improvements in patient safety.”
Dr. Emma Magavern, the lead author of the study in the BJCP, said, “The data all suggests that we can make prescribing safer for our patients by expanding the use of the PSA.”
More information:
Emma F. Magavern et al, UK Prescribing Safety Assessment (PSA): The development, implementation and outcomes of a national online prescribing assessment, British Journal of Clinical Pharmacology (2023). DOI: 10.1111/bcp.15919
Journal information:
British Journal of Clinical Pharmacology
Source: Read Full Article