A new preprint describes the significant variation in the early immune response elicited by two of the earliest vaccines to gain emergency authorization against coronavirus disease 2019 (COVID-19).
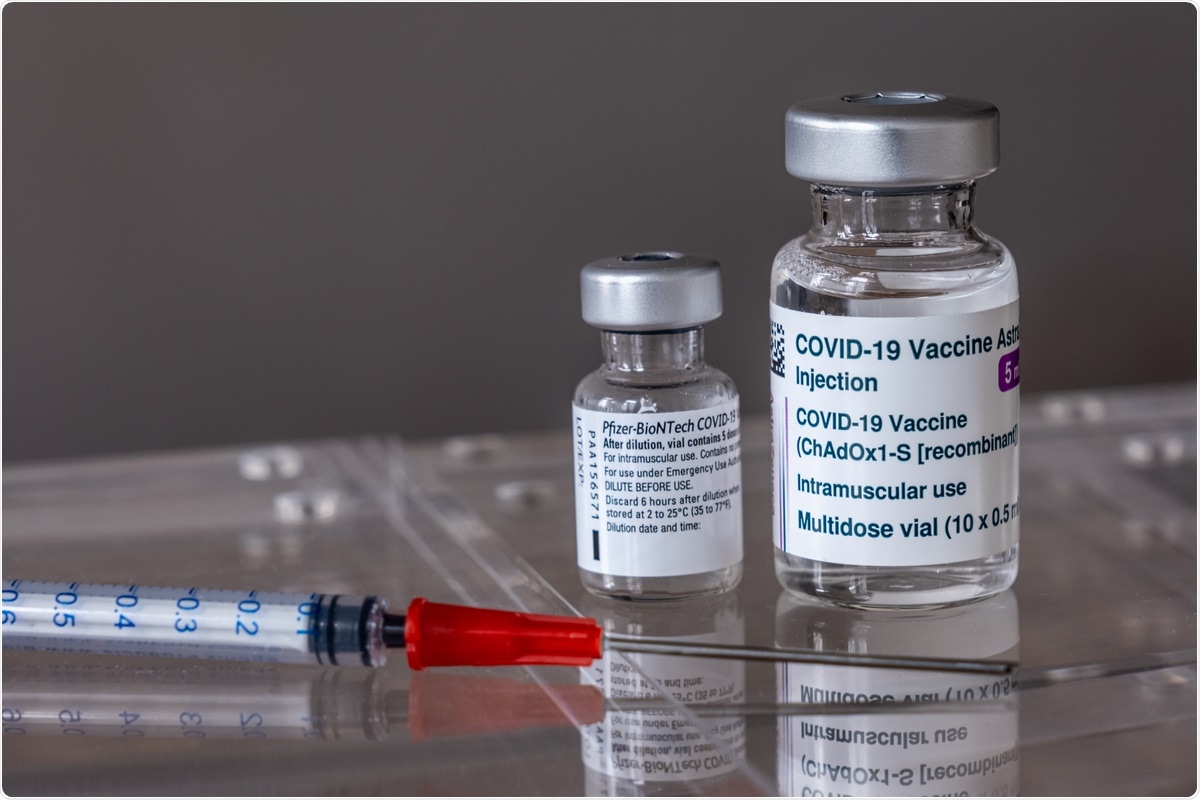 Study: Single-Dose SARS-CoV-2 Vaccination With BNT162b2 and AZD1222 Induce Disparate Th1 Responses and IgA Production. Image Credit: Marc Bruxelle/ Shutterstock
Study: Single-Dose SARS-CoV-2 Vaccination With BNT162b2 and AZD1222 Induce Disparate Th1 Responses and IgA Production. Image Credit: Marc Bruxelle/ Shutterstock
A preprint version of the study is available on the medRxiv* server while the article undergoes peer review.
Background
COVID-19 vaccination aims to elicit the production of antibodies that target the SARS-CoV-2 spike antigen, neutralizing its binding to the angiotensin-converting enzyme 2 (ACE2) receptor on the host cell to inhibit its entry into the host cell to establish infection.
The current study deals with two such vaccines:
- the first-generation adenoviral vector AZD1222 (from AstraZeneca) that utilizes the simian DNA adenovirus ChAdOx1 to deliver the virus spike into the vaccine recipient
- the Pfizer/BioNTech BNT162b2 vaccine based on messenger ribonucleic acid (mRNA) enveloped in lipid nanoparticles. The mRNA encodes the spike antigen for translation within the recipient cells.
Both these vaccines are linked to effective protection against symptomatic and severe COVID-19 after two doses. The earliest data points to high efficiency after one dose. Variants of the virus have emerged, with multiple spike mutations that cause greater loss of vaccine efficacy (VE).
The researchers wanted to explore the molecular and cellular immune responses occurring after one dose of either vaccine. Therefore, they studied the frequencies of various white blood cells in the peripheral blood involved in innate and adaptive immunity, tracing the changes in their numbers over the first three weeks from vaccination. They also looked at spike-targeting plasma immunoglobulin antibodies, in addition to the production and activity of spike-specific effector T cells.
What did the study show?
The researchers found that both vaccines produce different types and titers of antibody- and cell-mediated immune responses after one dose.
Early on, blood leukocytes dropped more than two-fold after one dose of the AZD1222 vaccine, mainly because of a decline in granulocytes, B cells, and CD4- and CD8-83 positive T cells. These counts were restored completely by day 13. Pro-inflammatory monocytes were also higher on day 2 in this group. With the granulocytes, CD14+CD16+ markers were elevated at this time.
Such changes were not recorded after the BNT162b2 vaccine, indicating that, unlike the AZD1222 vaccine, it did not cause much change in the number or frequencies of the innate immune cells, granulocytes, or monocytes.
At day 13 post-vaccination with BNT162b2, plasmablasts were found to peak with a median of 1.6%, compared to a day six peak with a median of 3% after the AZD1222 vaccine. Both CD27 and CD38 expression on CD8+ T cells were found to shift towards terminal differentiation of cytotoxic T cells at this time.
On day 20 also, CD4+CD127–CD27+effector memory T cells were observed to be higher in frequency, again indicating both B and T cell shifts after AZD1222 but not BNT162b2.
When white cells from COVID-19 convalescents or fully vaccinated individuals were stimulated by either the recombinant spike protein or the BNT162b2 spike-based vaccine, the former was found to cause CD4+ T cell activation. The latter led to the activation of both CD4+ and CD8+ lymphocytes.
Gamma-interferon (IFNγ)-producing cells were significantly increased after BNT162b2 vaccination but not with AZD1222.
Later responses
Adaptive responses after either vaccine showed that the immune response was also progressing to an effector T cell phenotype, with increased CD8+CD137+ T cells that also expressed the CD25 (IL-2Rα) marker. Spike-specific cytotoxic effector T cells were expanded as well, with higher proportions of FasL+CD8+ cells appearing after restimulation with spike mRNA.
The AZD1222 vaccine led to an increase in IFNγ-producing CD8+ T cells but reduced regulatory CD8+ cells and anti-inflammatory IL-2 and IL-10 co-production in.CD4+ and CD8+ cells alike.
Effector T helper cells were also increased with both vaccines, but only AZD122 was associated with increased pro-inflammatory TNFα-producing helper CD4+ T cells. Type 2 helper T cells specific to the spike antigen were conspicuously absent after either vaccine.
One dose of either vaccine thus led to a split in the CD4+ and CD8+ effector T cells, though the changes were more obvious after AZD1222.
Antibody responses
While AZD1222 predominantly induced IgM and IgG, with no detectable IgA production, up to day 20 post-vaccination, BNT162b2 elicited little IgM but higher increased IgG and IgA titers.
What are the implications?
The early immune reaction after a priming dose of either AZD1222 or BNT162b2 comprises strong cellular and antibody-mediated responses but with different patterns. While the former caused a drop in peripheral leukocytes on day 2, including granulocytes and B or T cells, it is attributable to the adenoviral vector. Other changes associated with AZD1222 also fit this picture, such as the transient increase in inflammatory monocytes.
The late-phase class switched response with memory B cells observed after one dose of this vaccine is known to be associated with high antiviral defenses. Thus, the adenoviral vector probably elicits these peripheral immune responses and not the SARS-CoV-2 spike antigen.
The BNT162b2 vaccination caused a less striking response, indicating that it is better tolerated. The vaccine mRNA has been designed to weaken its detection by innate immune cells. The small rise in frequency of plasmablasts after this vaccine may be due to adaptive immunity towards the spike protein, in contrast to the larger rise seen with AZD1222, elicited by the combination of adenoviral and spike-directed responses.
The strong IgA response with BNT162b2 vaccination may indicate the reason for its better symptomatic COVID-19 protection. Vaccine design should provide mucosal immunity to ensure IgA and tissue-resident effector cell activation to prevent infection at the nasopharyngeal mucosa.
While both vaccines expanded the effector T cells similarly, AZD1222 induced a Th1-skewed response, which may help drive a strong cellular immunity towards the spike antigen. Conversely, an overwhelming Th1 response may lead to a cytokine-secreting profile that inhibits class-switching towards IgA production.
However, BNT162b2 also induced IFNγ-producing T helper cells specific to the spike more strongly than AZD1222. Further research is needed to establish whether BNT162b2 promotes IgA production.
The Th1 response is common to both vaccines. The significant reduction in IL-10 may perhaps lead to a persistent Th1 response, setting up an environment that inhibits IgA production.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Müller, M. et al. (2021) "Single-Dose SARS-CoV-2 Vaccination With BNT162b2 and AZD1222 Induce Disparate Th1 Responses and IgA Production". medRxiv. doi: 10.1101/2021.09.17.21263726.
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Adenovirus, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Antigen, Anti-Inflammatory, Blood, CD4, Cell, Coronavirus, Coronavirus Disease COVID-19, Cytokine, DNA, Efficacy, Enzyme, Frequency, Immune Response, immunity, Immunoglobulin, Interferon, Nanoparticles, Phenotype, Protein, Receptor, Research, Ribonucleic Acid, SARS, SARS-CoV-2, Spike Protein, TNFα, Translation, Vaccine, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
