A blood test to watch breast cancer’s ‘molecular clock’ could help track the growth of multiple tumours around the body and monitor how they are responding to treatment, new research suggests.
The test could help identify the most actively growing tumours as breast cancer spreads around the body, helping to guide the best treatment for individual patients.
The approach has been developed following new results from an innovative rapid autopsy study, the LEGACY Study.
The new study found that the spread of breast cancer to multiple sites follows a traceable, orderly sequence, with the majority of new tumours in distant organs being formed by cancer cells all derived from one cell in the original breast tumour.
Highly sensitive and relatively cheap
While further development is required, scientists at The Institute of Cancer Research, London and The Royal Marsden NHS Foundation Trust believe the test would be highly sensitive and relatively cheap, as it doesn’t require prior knowledge of the genetic make-up of a patient’s cancer.
Secondary breast cancer is the term given to breast cancer that has spread to another part of the body, becoming incurable. Despite decades of progress, around 11,500 women in the UK each year still die from breast cancer, with almost all of these deaths being caused by secondary breast cancer.
It is estimated that around 35,000 people in the UK are living with secondary breast cancer. While secondary breast cancer can be controlled for some time, it currently cannot be cured and patients stay on treatment for the rest of their lives.
In a pilot rapid autopsy programme, led by consultant breast surgeon Peter Barry at The Royal Marsden, two women living with secondary breast cancer in London volunteered to donate their cancer tissue for research shortly after their deaths.
The LEGACY study, largely funded by Breast Cancer Now and sponsored by The Institute of Cancer Research (ICR) and The Royal Marsden, enabled researchers to remove and study secondary tumours rapidly after death.
Understanding how breast cancer cells evolve
As well as taking blood samples and biopsies from all the secondary tumours, whole lymph nodes were also removed, with all tissue being rapidly frozen at -80°C.
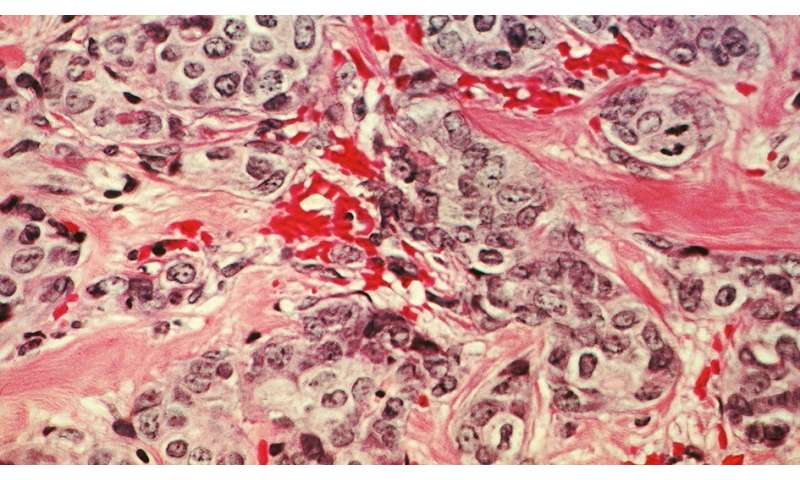
Researchers led by Professor Andrea Sottoriva at the ICR then studied the DNA from these secondary breast cancer cells, to try to gain a better understanding of how these cancer cells had changed over time.
The first LEGACY patient was a 51-year-old woman, who died 21 months after being diagnosed with de novo secondary breast cancer, meaning that the cancer had already spread from the breast to other parts of the body when she was first diagnosed.
The second LEGACY patient was a 35-year-old woman who was diagnosed with breast cancer during her pregnancy. After she had given birth, it was found that the breast cancer had spread to her bones and her lungs, and she died around 4 years after the initial diagnosis.
Ten of the twelve tumours found throughout the first patient’s body were found to have been established by ‘monoclonal seeding’, meaning that they originated from a single cell from the primary tumour in the breast.
In this patient, the breast cancer first spread to the lung, where a new tumour grew and evolved over time. The cancer cells from the lung tumour then seeded new tumours in the liver and ovary in two separate waves.
The tumour in the liver then also spread to the ovary and subsequently initiated a secondary tumour in the diaphragm. The ovary tumour also independently re-seeded the secondary tumour in the liver. Overall, only one liver and one ovary sample weren’t established by monoclonal seeding.
Monoclonal seeding was found to be the only way that breast cancer spread around the body in the second LEGACY patient. The researchers believe that if monoclonal seeding is the dominant way for breast cancer to spread, it could mean that tracking secondary breast cancer is more achievable than previously thought.
Developing a new kind of blood test
Professor Sottoriva’s team then went on to develop a new kind of blood test for cancer DNA to track how secondary breast cancer has spread.
Over time cells that actively grow and multiply accumulate molecular marks on their DNA, which appear in distinct patterns. The scientists found that by analysing cancer DNA fragments in the blood, it was possible to establish the ‘molecular clock’ of cancer cells that the DNA had come from, which identifies how many times they had multiplied.
By analysing these traceable ‘molecular clocks’ and comparing the blood test with the tumours collected during autopsy, the test built a family tree of the cancer cells, and the level of cancer cell DNA in the blood then provided information on which secondary tumours were the most active.
The researchers did however find defects in the way cancer cells were adding molecular marks to their DNA in the second patient, and so further research is needed to understand how common this challenge might be before a test for clinical use could be developed.
In addition, looking at data from an earlier study of eleven primary breast cancer patients whose disease had spread to the lymph nodes and for whom tissue and blood samples were available, the team confirmed that the ‘molecular clock’ blood test mirrored the genetic make-up of the tumour samples.
The authors propose that the blood test could be used to track how secondary tumours evolve over time, and to monitor their response to a range of treatments, including chemotherapy, immunotherapy or targeted therapies, as well as radiotherapy.
With further development, it is hoped that the ‘molecular clock’ blood test could also be used in the early detection of recurrence or spread following treatment, and may also be relevant for other forms of cancer.
‘Hope of effective treatment’
Professor Andrea Sottoriva, Director of Cancer Evolution in the new Centre for Cancer Drug Discovery at The Institute of Cancer Research, London, said:
“Our study sheds light on two of the central challenges in cancer research and treatment—cancer’s lethal ability to adapt and evolve, and its tendency to spread outwards from the initial tumour to other parts of the body.
“The LEGACY study gave us a unique opportunity to analyse the genetic make-up of breast cancer after it has spread to multiple sites in the body, shedding new light on the course of cancer evolution.
“We also identified a brand new way of understanding how the tumour grows and evolves, through analysing ‘molecular clock’ signatures from cancer DNA in the blood.
“We hope to develop a blood test to monitor the evolution of an individual patient’s cancer, and in doing so, to offer hope of effective treatment even where there has been extensive cancer spread.”
Peter Barry, Surgical Oncology lead for the Breast Cancer Now LEGACY Study, and Consultant Breast Surgeon at The Royal Marsden, London, said:
“This was a wonderful result of collaboration with a highly innovative team in the ICR led by Professor Sottoriva. It points the way to potentially sample one active metastatic site in a patient and then using the molecular clock signature with regular blood tests, test and monitor new treatments in real-time.
“Clearly we need to expand this testing to a larger cohort of patients to see how widely applicable it might just be—in breast cancer patients as well as potentially in patients with other cancer types. I am wholeheartedly grateful to the patients and their families who so generously made this study possible.”
‘Made possible thanks to the patients’ selfless donations’
Dr. Simon Vincent, Director of Research, Support and Influencing at Breast Cancer Now, which funded the study, said:
“Studying how and why breast cancer spreads through the body is vital if we are going to find a way to stop it. This innovative study, made possible thanks to the patients’ selfless donations, helps us gain insight into how breast cancer spreads from one part of the body to another, paving the way for further research to stop secondary breast cancer.
“The development of a blood test to continuously track how a patient’s cancer is changing and responding to treatment is an exciting step towards being able to offer patients a more personalised treatment plan which could be readily adapted if a certain therapy is no longer effective. However, for this blood test to reach clinics, more testing and refinement in a larger number of people is now required.
Source: Read Full Article
