It may not receive the same attention as the heart or brain, but a diseased kidney can be more deadly, with effects that weaken the heart, bones, and immune system, let alone the kidney itself. End-stage kidney disease has the worst prognosis, and the only curative option is a kidney transplant, which comes with its own risks. A collaboration between Kyoto University and Akita University, Japan, and led by ASHBi Professor Motoko Yanagita has found a common but previously unappreciated observation of kidney grafts, tertiary lymphoid tissues, is a valuable prognosis marker of the graft outcome. The new study can be seen in the Journal of the American Society of Nephrology.
There were nearly 100,000 kidney transplantations done last year, ten times the number of heart or lung transplants. Moreover, five of every six patients waiting for an organ donor are in need of a kidney transplant. Even if a donor is found, however, there is no guarantee that the patient will be cured.
“Graft survival in the short-term has greatly improved in the last three decades, but long-term survival has only improved marginally,” said Yanagita, who is an expert of kidney disease.
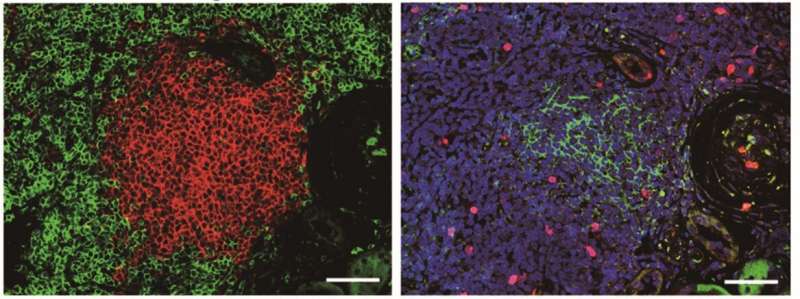
One of the key indicators of a failing transplant is inflammation. Commonly accompanying the inflammation are tertiary lymphoid tissues, which the study describes as “inducible ectopic lymphoid tissues that arise in chronic inflammatory conditions such as aging, cancer, autoimmune disease and transplanted organs.”
In other words, tertiary lymphoid tissues are a natural development of aging and the associated health burdens that come with it. However, while the medical community is well aware of the appearance of tertiary lymphoid tissues in kidney transplants, there is little understanding about their role in graft survival.
One reason the significance of tertiary lymphoid tissues had been ignored was that doctors and scientists had not appreciated the different stages of the tissues. Last year, Prof. Yanagita’s team reported two stages distinguished by the absence (stage I) and presence (stage II) of follicular dendritic cells, a natural type of fibroblasts found in the human body.
The new study examined 214 kidney transplant patients who showed no rejection. Each patient underwent kidney biopsies immediately, 1, 6 and 12 months after the transplantation to ensure no rejection. Tertiary lymphoid tissues were hardly seen immediately after the transplantation but were already present in about half after one month.
Stage II tertiary lymphoid tissues, however, were only found in less than 10% of biopsies after 6 months and in almost 20% after one year. Yet those patients whose biopsies showed stage II tertiary lymphoid tissues also had a much higher likelihood of renal failure within five years of the transplantation.
“The patients with stage II tertiary lymphoid tissues showed a higher risk of future decline in graft function,” said Yanagita.
Moreover, she added, the presence of stage II tertiary lymphoid tissues did not necessarily associate with the inflammatory score of Banff classification, a standard scoring system used by clinicians to grade biopsies from solid organ transplants. Instead, the stage II tertiary lymphoid tissues may provide another useful diagnostic marker of graft survival in kidney transplantation.
Source: Read Full Article
