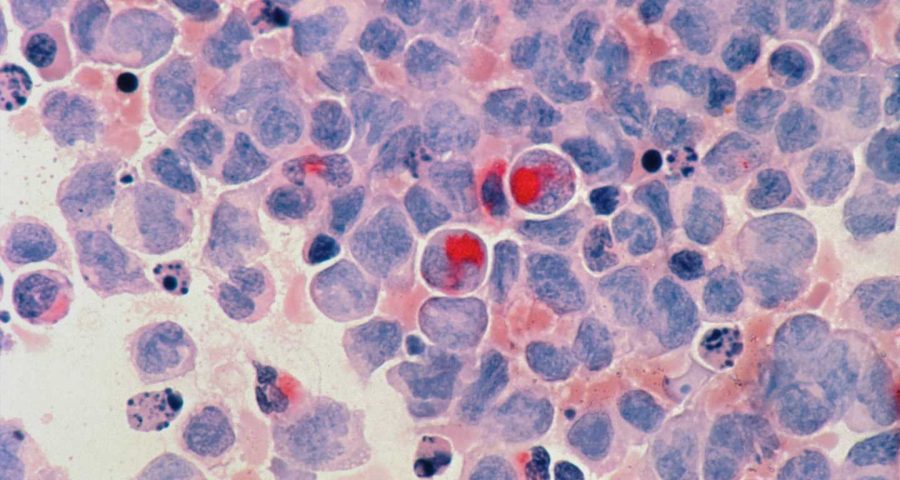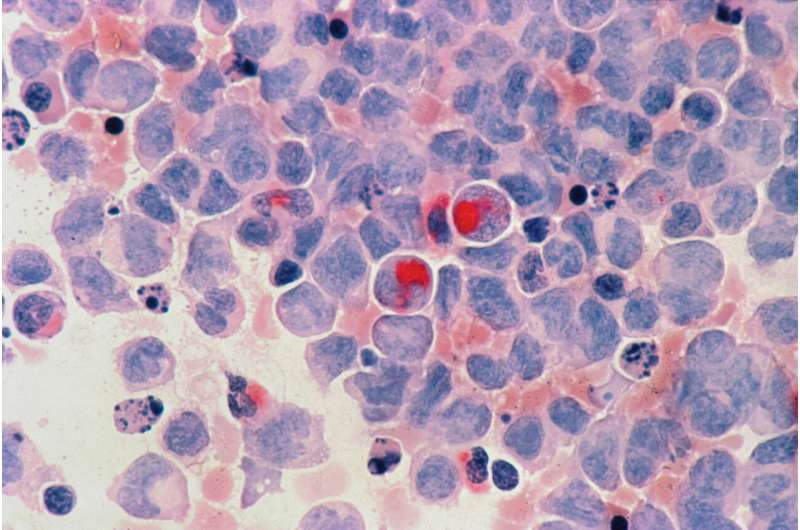
Scientists at St. Jude Children’s Research Hospital developed a strategy to improve the ability of engager (ENG) T cells to kill acute myeloid leukemia (AML). The approach showed promise in preclinical models against hard-to-treat relapsed disease. The results were pre-published today in the journal Haematologica.
Despite advances in pediatric leukemia treatment, clinical outcomes remain poor for relapsed AML. Researchers are exploring multiple potential therapies. One approach uses ENG T cells. These cells are immune cells that have been modified to secrete antibodies that bring T cells and cancer cells together, promoting tumor killing. Scientists at St. Jude developed a way to improve on ENG T cells, making the therapy more efficient and effective. They added a co-stimulation system controlled by an activating drug to the ENG construct. Preclinical findings show that the approach increased the anti-AML activity of ENG T cells.
“We’re basically having the T cells express a battery that we can control,” said corresponding author Paulina Velasquez, M.D., St. Jude Department of Bone Marrow Transplantation and Cellular Therapy. “ENG T cells secrete a protein that allows the T cells to kill leukemia. In this case, when they also express the controlled battery that we added, we are getting extra mileage out of these cells.”
ENG T cells for AML improve with inducible co-stimulation
Regular ENG T cells quickly become exhausted after encountering tumor cells, ending their therapeutic effect. The St. Jude team found that co-stimulation can counteract exhaustion, making the ENG T cells work better. The team tested inducible co-stimulatory proteins that only function in the presence of a small molecule (drug). The drug gives the researchers more control, even after the ENG T cells are infused into a patient. In addition to preventing exhaustion, this system can serve as an important safety feature because the inducible co-stimulation can be easily curtailed if the drug is stopped.
Velasquez and her team tested whether expression of inducible co-stimulatory proteins that activate MyD88, CD40, or both MyD88 and CD40 immune pathways in ENG T cells improves their antitumor activity. AML-specific ENG T cells in which both signaling pathways were activated outperformed their unmodified counterparts or ENG T cells in which only one of the pathways was active in laboratory studies as well as animal models.
ENG T cells: A promising alternative to treat relapsed AML
At present there are many genetic approaches to render T cells specific for AML. This includes, for example, expression of chimeric antigen receptors (CARs). In contrast to CAR T-cell therapy for acute lymphoblastic leukemia (ALL), the clinical experience with AML-specific CAR T cells has presented challenges.
Source: Read Full Article