A dysregulated and weak immune system can affect the severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. The function and regenerative ability of dendritic cells (DC) and monocytes can have an effect on the immunopathology and adaptive immune response to SARS-CoV-2, the virus responsible for the COVID-19 pandemic.
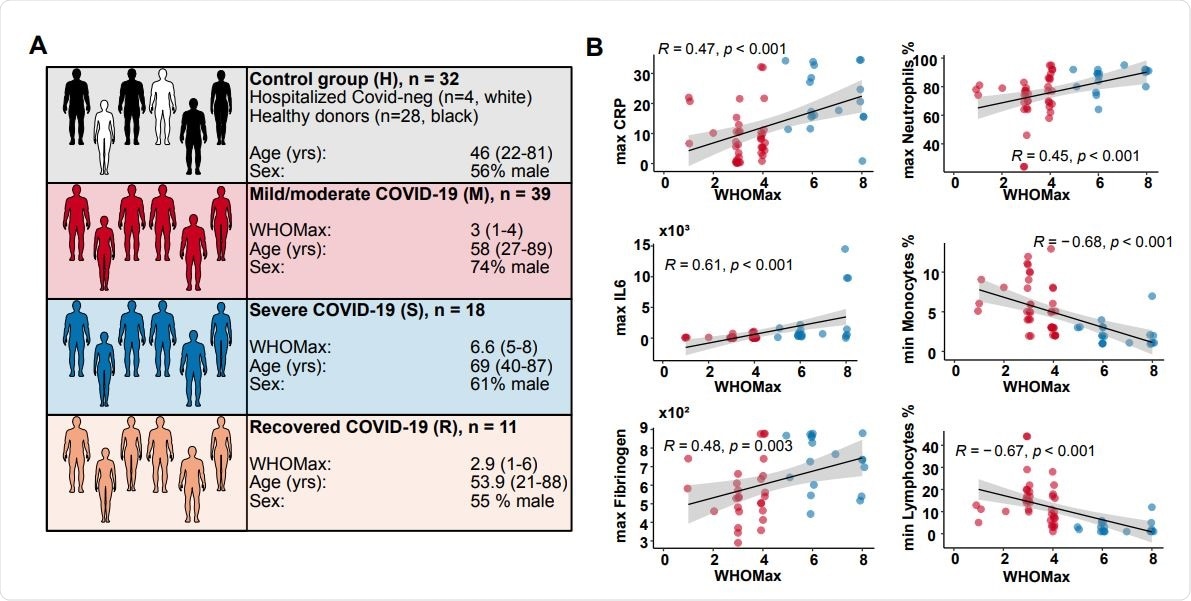
A group of researchers from Germany has investigated and analyzed circulating dendritic cells and monocyte subsets in 65 hospitalized COVID-19 patients with mild to severe presentations of the infection. A variety of patients were included in their study, from those who exhibited minor signs of acute disease to convalescents, as well as healthy controls.
A pre-print version of the research paper is available on the bioRxiv* server, while the article undergoes peer review.
Dendritic Cells
Dendritic cells work as highly efficient antigen-presenting cells and are essential to the immune system. They provide an essential service by recognizing pathogens while also playing a significant role in both the innate and adaptive immune responses as well as secreting inflammatory mediators.
The various DC subpopulations play a different role in the antiviral immune response. Conventional DCs (cDC) are effective in presenting antigens as well as leading naïve T cells into expanding and differentiating. The cDC1 population type has an affinity for cross-presentation of antigens to CD8+ T cells, while cDC2 influences T helper cell responses.
Research into conventional DCs within COVID-19 patients has found that in severe cases of the SARS-CoV-2 infection, there has been an overall reduction of cDC subsets in the blood as well as an accumulation of activated cDC2 found in the lungs. Plasmacytoid dendritic cells (pDC), which work to rapidly produce antiviral type I interferons and inflammatory chemokines, have also been found in COVID-19 patients to have a reduction in numbers as well as also lack functionality.
Additionally, monocytes, which are usually recruited to inflammatory sites and have the ability to differentiate into macrophages and monocyte-derived DCs, have been found to work differently within COVID-19 infections. Their recruitment to inflammatory sites during a SARS-CoV-2 infection causes subsequent proinflammatory cytokines to be produced which can contribute to the advancement of the infection as well as tissue damage.
The Study
The aim of this study was to gain an in-depth understanding of the changes in dendritic cell frequency, activation status, and functionality within the adaptive immune response and within the severity of disease among COVID-19 patients.
The researchers observed a lasting reduction of dendritic cell subpopulations in COVID-19 patients while also finding an expansion of proliferating immune cells (HLADR+ lineage cells) which lack DC markers and also lack regeneration.
Study results also revealed dysregulated activation patterns including an early type I interferon-induced response as well as others, and this could be linked to a reduced ability to stimulate T cells, a sign of being infected more severely with SARS-CoV-2.
Significance for COVID-19 Patients
The impaired functionality and reduction of dendritic cell numbers in COVID-19 patients affect the ability of DCs to stimulate naïve T cells in order for them to respond appropriately to the infiltration of SARS-CoV-2 within the body. Due to inefficient and inadequate adaptive immune responses, patients may present with more severe cases of infection if they are unable to clear the virus.
While the researchers found the frequency of activated T cells to be variable in the sample observed, a subgroup of patients compared to the control group did have reduced T cell activation. Due to there being some contrast in responses for other viral infections or in those vaccinated, it may be possible that the reduction in T cell activation may only be in those recruited to the site of the airways as opposed to circulating T cells around the body, and this may require more research.
Other research developments that the study mentions that may also be required include the dysregulated activation of DCs and if they influence the activation of T helper cells and B cells, as well as if both are affected by long-lasting inflammatory responses against SARS-CoV-2.
The study examined how COVID-19 might affect the role of dendritic cells, and it concluded that because the infection can deplete the number of this essential immune cell, patients may be more susceptible to secondary infections, and their health may have to be managed more carefully.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Winheim, E., Rinke, L., Lutz, K., Reischer, A., Leutbecher, A., Wolfram, L., Rausch, L., Kranich, J., Wratil, P., Huber, J., Baumjohann, D., Rothenfußer, S., Hellmuth, J., Scherer, C., Muenchhoff, M., Bergwelt-Baildon, M., Stark, K., Straub, T., Brocker, T., Keppler, O., Subklewe, M. and Krug, A., 2021. Impaired function and delayed regeneration of dendritic cells in COVID-19. DOI: https://doi.org/10.1101/2021.05.26.445809, https://www.biorxiv.org/content/10.1101/2021.05.26.445809v1
Posted in: Medical Research News | Disease/Infection News
Tags: Antigen, Blood, Cell, Chemokines, Coronavirus, Coronavirus Disease COVID-19, C-Reactive Protein, Cytokines, Dendritic Cell, Frequency, Immune Response, Immune System, Laboratory, Lungs, Monocyte, Pandemic, Protein, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Virus

Written by
Marzia Khan
Marzia Khan is a lover of scientific research and innovation. She immerses herself in literature and novel therapeutics which she does through her position on the Royal Free Ethical Review Board. Marzia has a MSc in Nanotechnology and Regenerative Medicine as well as a BSc in Biomedical Sciences. She is currently working in the NHS and is engaging in a scientific innovation program.
Source: Read Full Article
