In a recent study published in the Canada Communicable Disease Report, researchers assessed the hospital and associated resource costs related to antimicrobial-resistant (AMR) infections in Canada.
Background
AMR is a severe and expanding health concern in Canada and across the globe. This phenomenon is noted when microorganisms become resistant to treatment by either first-line or standard antibiotic drugs. Recently, more microorganisms have exhibited resistance to currently used antibiotics as well as novel antimicrobials. This has led to increased infection cases because of previously treatable diseases.
Such infections create a huge burden on the patients as well as society as related morbidity and mortality increase. Additionally, AMR elevates the burden faced by the healthcare system due to longer hospital stays and the demand for more expensive resources and therapies, which could be employed to treat other diseases.
Valid information related to the costs associated with AMR could provide valuable data on the extent of its burden while addressing the gaps in knowledge and providing inputs and evidence for policy assessment.
About the study
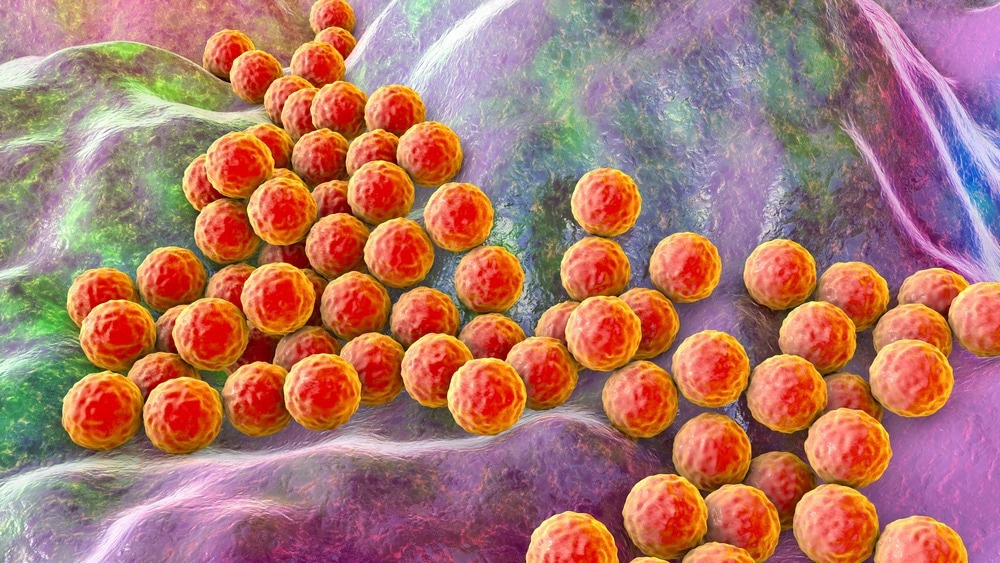
In the present study, researchers estimated the hospital costs related to two important antibiotic-resistant organisms namely, Clostridioides difficile (C. difficile) and methicillin-resistant Staphylococcus aureus (MRSA), in Canada in 2019.
The team utilized the Discharge Abstract Database (DAD) obtained from the Canadian Institute for Health Information as the main source of study data. The DAD comprises administrative information on hospital discharges, patient characteristics, diagnoses, and facilities provided in all territories and provinces. The team also collected data related to the cost associated with a standard hospital stay and the resource intensity weight related to each hospital discharge. All analyses conducted employed the data between 2010 and 2019. Analysis was performed on individuals aged 18 years and older.
For each separation reported, the DAD included up to 25 possible diagnoses as per the International Classification of Diseases (ICD)-10 codes. Each record noted the most responsible diagnosis (MRDX), the condition or diagnosis that could be described as the most responsible cause for the patient’s hospital stay. If more than one of such conditions were found, the one assumed to be most responsible for the longest portion of the patient’s length of stay (LOS) or the greatest utilization of resources was chosen.
Costs and incidence of MRSA infections were categorized into non-bloodstream (non-BSI) and bloodstream (BSI) infections. Costs and incidence of C.difficile infections (CDI) were evaluated separately for cases in which C. difficile was either the most responsible or the secondary diagnosis. Additionally, the team estimated the increased mortality attributable to the infection assessed to evaluate the value of lost production because of premature mortality due to AMR infections.
Results
The study findings showed that the incidence of CDI had reduced from 7.1 cases per 1,000 hospital separations in 2015 to 5.8 cases per 1,000 hospital separations in 2019. Assessing the methicillin-resistant as well as the Staphylococcus infection diagnoses showed that all the cases in 2010 had both diagnoses, while 85% belonged to the same cluster.
Furthermore, 76% of infections diagnosed as methicillin-resistant and having a BSI with Staphylococcus were in the same cluster. In 2019, the overall MRSA incidence rate was 3.6 per 1,000 separations, including 2.6 and 1.0 for non-BSI and MRSA-BSI, respectively.
The team also noted that patients having any infection type had a much longer average LOS. Furthermore, patients with CDI were more likely to be older, while those with MRSA infections were younger. Males had a higher chance of being diagnosed with MRSA infection than females. Also, individuals aged 75 years and more displayed the highest overall rates. However, MRSA infection rates were the highest for those aged between 35 and 54.
The unadjusted costs were comparatively high and ranged between $19,000 per non-BSI and MRSA patient and $30,000 per CDI patient. This was perhaps because AMR patients have longer LOS with more resource utilization.
The average incremental expenditures across all age cohorts were $2,301 for non-BSI MRSA infections and $3,654 for BSI MRSA infections. This resulted in a total hospital cost associated with MRSA of $24.4 million. On the other hand, the average cost per CDI patient was $11,056, while the incremental costs for secondary CDI were $3,749. This totaled the CDI-related hospital costs to almost $100.7 million.
The team estimated that the number of deaths due to CDI was 1309, MRSA non-BSI was 257, and MRSA BSI was 177. Most of the estimated mortalities were observed between patients aged 75 years and above. Furthermore, AMR infections led to 1743 extra mortalities and were responsible for total economic costs ranging from $143.8 million to $272 million.
Conclusion
Overall, the study findings showed that estimating the outcomes related to AMR infections provided valuable data for policymakers. The researchers believe that this quantification is an important step in understanding the economic effects of AMR.
-
Diener A, Wang H, Nkangu M. Hospital and related resource costs associated with antimicrobial-resistant infections in Canada, 2019. Can Commun Dis Rep 2022;48(11/12):529–39. doi: https://doi.org/10.14745/ccdr.v48i1112a06
https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2022-48/issue-11-12-november-december-2022/hospitals-related-costs-associated-antimicrobial-resistant-infections-canada-2019.html
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibiotic, Communicable Disease, Drugs, Healthcare, Hospital, International Classification of Diseases, Mortality, Staphylococcus aureus

Written by
Bhavana Kunkalikar
Bhavana Kunkalikar is a medical writer based in Goa, India. Her academic background is in Pharmaceutical sciences and she holds a Bachelor's degree in Pharmacy. Her educational background allowed her to foster an interest in anatomical and physiological sciences. Her college project work based on ‘The manifestations and causes of sickle cell anemia’ formed the stepping stone to a life-long fascination with human pathophysiology.
Source: Read Full Article
