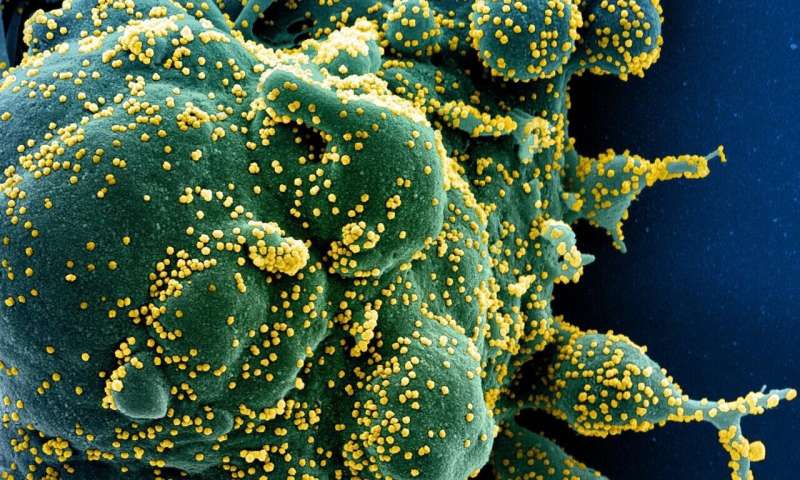
Recent studies have shown that immune response plays a central role in the severity of COVID-19. Understanding the immune responses generated as the disease progresses is therefore key to determining which patients are at highest risk of developing serious complications or dying as a result.
In a study published Feb. 26 in the Journal of Clinical Investigation, scientists and clinicians led by Université de Montréal neuoscientist Dr. Catherine Larochelle, a researcher at the Centre hospitalier de l’Université de Montréal Research Centre, have shown that a set of immune alterations are specifically linked to infection with the SARS-CoV-2 virus.
The research team also found the alterations are linked to the severity of COVID-19 disease, to its evolution over 30 days, and to death within 60 days. These biomarkers could represent potential therapeutic targets, according to Larochelle, the principal author of the study.
She spoke to us about her findings.
Your experimental approach is rather unique. Based on the immune profiling you conducted, how were you able to identify the patients most at risk for a poor prognosis?
Above all, this is the result of a tremendous collective effort by several dozen people involved in research and clinical work at the CHUM, who participated in this study and in the Quebec COVID-19 (BQC19) Biobank.
Based on a blood test, we were able to inventory the immune-cell populations present in 50 patients with SARS-CoV-2 and compare them to those of 22 patients of similar gender and age hospitalized for other acute illnesses, and those of 49 healthy controls.
This immune profiling allowed us to identify subsets of “dysregulated” immune cells specific to patients affected by SARS-CoV-2. Most notably, some of these immune alterations were associated with ventilation needs and mortality in these same patients.
These markers specific to SARS-CoV-2 could then help us to identify the patients at greatest risk, and suggest new avenues for developing therapeutic targets.
In addition, we confirm what has been observed in other studies: disturbances in the immune system such as neutrophilia or lymphopenia, for example, are related to the severity of the disease in hospitalized patients, but are not specific to SARS-CoV-2.
From a clinical perspective, this could explain why general anti-inflammatory treatments such as steroids seem to work in COVID-19 and other acute diseases.
How do you see your results being used directly in a clinical setting? Is it technically feasible?
These assays could be easily transferred to clinical settings, because we worked with very small amounts of blood—less than one milliliter—to develop these immune profiles.
In our experimental approach, we used techniques commonly employed in hospital laboratories: using surface antibodies to “stain” the cells that express certain markers, flow cytometry (cell characterization and counts), etc. In a clinical setting, this could help track the progress of patients over time and ultimately identify those at high risk who would require closer monitoring.
What therapeutic horizons do you envision for your research work?
Source: Read Full Article
